Acute pancreatitis post-ERCP
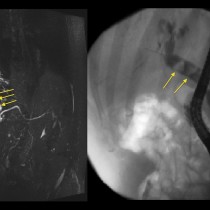
This patient presented with jaundice that was caused by a pancreatic tumour obstructing his common bile duct (CBD). He underwent an endoscopic retrograde cholangiopancreatography (ECRP) at which time a plastic CBD stent was inserted. The next day he was complaining of abdominal pain. Serum amylase was elevated and a CT was requested.
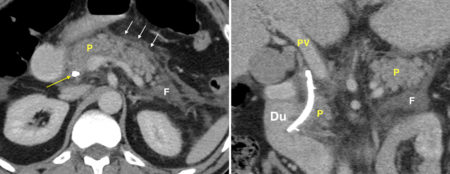
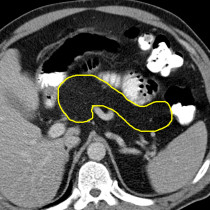
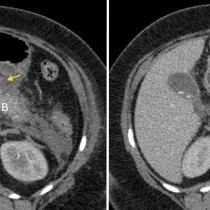
The transverse CT image on the left shows the plastic stent (yellow arrow) passing through the head of the pancreas (P). There is stranding of the fat anterior to the pancreas, white arrows, and there is retroperitoneal fluid adjacent to the body and tail of the pancreas (F). The coronal CT image on the right shows the CBD stent more clearly, passing through the ampulla into the duodenum (Du). Again, there is haziness of the fat around the pancreas (P) and fluid in the adjacent retroperitoneum (F). ‘PV’ = portal vein.
These are typical CT features of acute pancreatitis, which in this case was a complication of the ERCP.
There was no pancreatic necrosis and the patient’s symptoms settled rapidly with conservative management. He subsequently underwent a Whipple procedure to resect the pancreatic tumour.
Acute pancreatitis is one of the most feared complications of ERCP, as it has a high morbidity and a mortality rate of approximately 1-3%1. It occurs in around 5% of patients who undergo ERCP, and is more common in female patients and those have a past history of pancreatitis. With the widespread availability of a non-invasive means of imaging the biliary tree and pancreatic duct (magnetic resonance cholangiopancreatography, or MRCP), ERCP is now reserved for patients who require intervention, for example sphincterotomy, CBD stone extraction, CBD or pancreatic duct stent insertion, or brushings of the CBD when malignancy is suspected.
Reference:
Donnellan F. Prevention of post-ERCP pancreatitis. Gastroenterology research and practice 2012. http://dx.doi.org/10.1155/2012/796751