Xanthogranulomatous pyelonephritis (XGP)
This diabetic woman in her 60s presented with vague flank discomfort and recurrent fevers and was referred for an ultrasound, on the basis of which a CT urogram was requested.
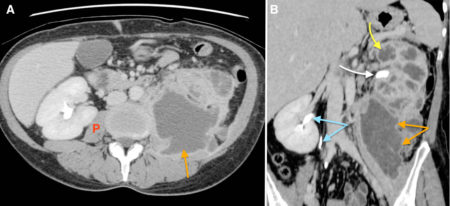
These images are taken from the delayed phase of the CT and show a normal right kidney but a grossly abnormal left kidney, with a large calculus in the renal pelvis on this side (white arrow, image B). IV contrast has been excreted into the renal pelvis and ureter on the right side (blue arrows) but not on the left, indicating that this is a poorly- or non-functioning kidney.
The calyces in the left kidney are dilated (the low density structures on image B, one of which is indicated by the yellow arrow).
There is an abscess-like inflammatory process extending from the affected kidney into the perinephric fat and infiltrating the left psoas muscle (orange arrows on both images – compare with normal right psoas labeled ‘P’ on image A).
This appearance is typical of a condition called xanthogranulomatous pyelonephritis, or XGP.
XGP is a rare disease caused by chronic granulomatous infection of the renal pelvis, usually in the setting of an obstructing calculus (often a staghorn calculus). It is more common in women and in diabetics, and most frequently affects the 45-65 year-old age group although patients can be affected at any age including in infancy.
The renal calyces become filled with pus and debris, while the renal parenchyma is infiltrated and eventually replaced by the associated inflammatory response (characteristically containing lipid-laden macrophages or ‘xanthoma’ cells, which is where the name XGP comes from). The CT appearance of the dilated, low density calyces contrasting with the adjacent renal parenchyma has been likened to a bear’s paw. The inflammatory process frequently extends outside the kidney, invading the surrounding fat and musculature as well as, occasionally, the spleen and colon.
The treatment for XGP is nephrectomy.