Ischaemic colitis – CT
This 75 year old man presented to the ED with abdominal pain, diarrhoea and rectal bleeding and was referred for an abdominal CT.
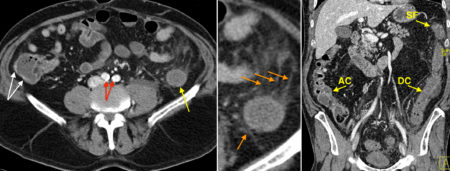
On the transverse contrast-enhanced CT image on the left, you can see normal enhancement of the wall of the ascending colon (white arrows). However, the wall of the descending colon doesn’t enhance and is around the same density as the fluid in its lumen (yellow arrow). There is inflammatory change in the surrounding fat, which is hazy and contains some linear strands of increased density, indicated by the orange arrows in the middle zoomed image. On the right is a coronal image which nicely illustrates the difference between the walls of the right and left colon, with normal enhancement of the wall of the ascending colon (AC) but diffusely reduced enhancement of the colonic wall from the splenic flexure (SF) to the distal descending colon (DC). The wall of the affected descending colon is also thickened, and the sigmoid colon (not shown) was similar in appearance.
This patient also shows evidence of underlying atherosclerosis, with calcification in the iliac arteries (red arrows).
The findings of reduced mural enhancement, wall thickening and adjacent fat stranding in the colon of an elderly patient, especially in this distribution, are consistent with ischaemic colitis, which would also fit with the patient’s clinical presentation.
Ischaemic colitis usually occurs in elderly patients (over the age of 60) with underlying atherosclerosis. Precipitating events in these patients include hypoperfusion caused by heart failure, hypotension (for example, in sepsis) and hypovolaemia. Arterial emboli, for example in patients with atrial fibrillation, can also result in colonic ischaemia. There is a wide spectrum of severity of ischaemic colitis, from mild and transient (often subclinical), to severe and fulminant, where irreversible ischaemia occurs. In some patients, the ischaemia is mild but recurrent and results in colonic strictures that may cause obstruction.
In the majority of patients, ischaemic colitis is transient and reversible, and involves the left side of the colon (inferior mesenteric artery territory, from splenic flexure to upper rectum, as in this example).
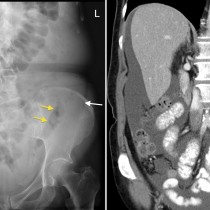
Plain film of the abdomen (PFA) in patients with ischaemic colitis is usually normal. Occasionally, the affected colonic segment will be mildly dilated, and sometimes the wall thickening will be visible as ‘thumb printing’ (see an example of this here). If irreversible ischaemia occurs, necrosis of the colonic wall can result in gas within the wall (pneumatosis).
In most patients, CT is required for diagnosis and will show the typical features illustrated in this example. In severe cases, pneumatosis, portal venous gas, perforation or complete occlusion of the superior or inferior mesenteric artery may be seen.