Embolization for GI haemorrhage
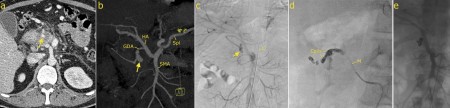
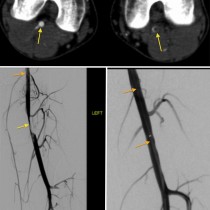
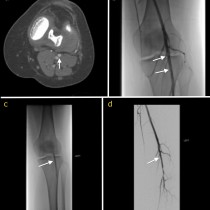
Embolization for GI haemorrhage. This 44 year old man presented to ED with haematemesis and melaena, and his haemoglobin rapidly dropped from 10.3 to 6.5. A CT was performed and showed stranding of the fat around the duodenum, suggesting either duodenitis or a penetrating ulcer. The rounded focus of enhancement adjacent to the duodenum on image (a), arrow, is a pseudoaneurysm of the gastroduodenal artery, which was the source of the haemorrhage. These are recognized complications of peptic ulcer disease and pancreatitis. Image (b) is a maximum intensity projection (MIP) from the CT, showing the pseudoaneurysm (arrow) as well as the normal arterial anatomy (GDA: gastroduodenal artery, HA: hepatic artery, Spl: splenic artery, SMA: superior mesenteric artery). The patient was transferred to IR. Image (c) shows a catheter, ‘C’, which has been advanced into the coeliac artery. Contrast injection shows the pseudoaneurysm (arrow). A microcatheter (less than half a millimeter in diameter, ‘M’ on image (d)) is advanced into the GDA and embolization coils inserted in order to occlude the artery. Post-procedure angiogram, (e), shows no residual flow in the GDA. The patient stabilized and the haemorrhage did not recur.