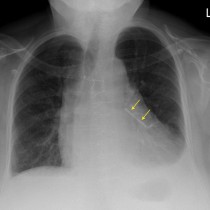
Renal infarct secondary to atrial fibrillation
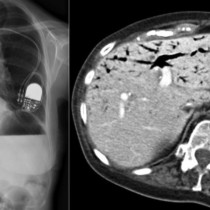
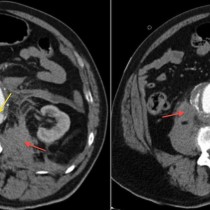
This 60 year old man presented to the ED with sudden onset right iliac fossa pain. Initial work-up in the ED revealed that he had atrial fibrillation, not previously diagnosed. As embolisation of thrombus related to the atrial fibrillation was suspected to be the cause of the abdominal pain, a dual-phase (arterial and portal venous) CT of the abdomen was performed as this helps to identify changes of ischaemia. The CT showed a wedge-shaped area of absent perfusion in the right kidney – this is the low attenuation area outlined by the yellow lines on the transverse (left) and coronal (right) CT images here. These images are from the arterial phase – note the intense high density in the abdominal aorta and, immediately anterior to it, the superior mesenteric artery.
In patients with atrial fibrillation and abdominal pain, CT may identify infarcts in the kidneys, spleen, gallbladder and bowel. The liver is protected due its dual source of blood supply from the hepatic artery and portal vein.
In patients with atrial fibrillation who have been anti-coagulated, acute abdominal pain may be due to haemorrhage rather than ischaemia. Patients may bleed into the bowel wall instead of the lumen, which results in high attenuation thickening of the wall and may rupture into the peritoneal cavity, causing haemoperitoneum. Haemorrhage may also occur into the urinary tract, potentially causing ureteric obstruction (‘clot colic’). Anti-coagulated patients occasionally develop spontaneous haemorrhage into abdominal muscles, particularly the rectus abdominus and the psoas major, which also present with pain.